It is well known that CT procedures provide valuable and irreplaceable diagnostic information for patients. CT volumes are on the rise— with more than 62 million scans performed each year. However, with this increase in utilization, there is a growing concern about the cumulative radiation dose to the general population.
A recent article in the “Journal of the America College of Radiology/Vol. 9 11 November 2012 by John O. Johnson, MD and Jon M. Robins, MD” provided a thorough examination of the risks of CT Radiation Doses and the strategies that are being incorporated to combat that risk. While it’s impossible to provide you with all of the valuable information in the article, here are some of the highlights. However, any CT provider should review the article in its entirety. It’s a great resource to help you prepare for 2013 and beyond.Increased scan volumes equate to increased radiation exposure to the general population. Unfortunately, that also theoretically equates to increased cancer risks to those receiving CT scans. In fact, 0.7%-2.0% of future cancers may be attributable to CT scans. This risk increases for children, since they are more radiation sensitive and have longer post radiation life spans. With four million CT scans being performed on children each year, concerns about radiation exposure are warranted. For every 1,000 patients that receive a 10-mSv exposure, one excess cancer can be predicted.
As a result, radiation specialists have recognized the need to minimize radiation dose exposure during CT scans. They are quickly adopting new strategies to reduce patient dose while maintaining diagnostic image quality. The good news is that these new strategies can be simple, reproducible and inexpensive to implement.
New radiation dose reduction strategies include:
- Redesigning CT acquisition protocols
- Adjusting CT doses based on each patient’s Body Mass Index (BMI)
- Limiting the length of CT scan coverage
- Revisiting how we administer multi-phase examinations
- Implementing iterative reconstruction hardware/software
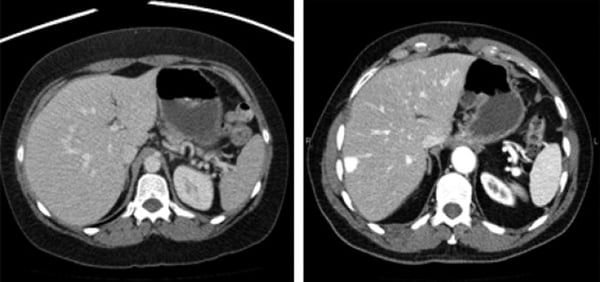
Fig 1. Peak kilovoltage, 120 kVp vs 100 kVp. The image on left was obtained at standard 120 hVp. The axial image on the right was obtained at 100 kVp. Note comparable image quality with expected increased image contrast at reduced peak kilovoltage.
Let’s take a look at some specifics outlined in this informative article.
Decreased Peak Kilovoltage is very valuable tool, but can be tricky because changing kilovoltage (kVp) has a non-linear effect on radiation dose reduction. For example, while “normal” kVp for an adult is 120, we also know that adults vary in size. However, by using a patient’s Body Mass Index (BMI) to determine the patient size, you can accurately adjust and optimize kVp to maximize dose reduction.
Automatic Dose Modulation: Most all-modern CT scanners have the ability to automatically adjust x-ray tube current (mA) on the basis of each patient’s size and shape (auto-mA). It’s important to have an understanding of the amount of noise allowed for defining auto-mA parameters, depending on the vendors and types of CTs you use. As noise allowance is increased, the mA and dose are decreased. Having an understanding of the relationship between allowed system noise and how it effects auto-mA and dose will allow you to increase the amount of noise used for auto-mA and to decrease mA and patient dose—all while maintaining diagnostic image quality. Just remember, the noise values may be different on each type of scanner you use, plus each scanner must be “tuned” to achieve the required dose reduction goals.
Decreased Length of Scan Coverage: The length of CT acquisition is directly proportional to CT dose. Because of this, it is important to limit the length of each scan (z-axis) and the number of phases (arterial, venous, delayed) so that only the anatomy of clinical interest is included in the scan.
Pitch: It’s important to evaluate pitch adjustments. The faster the pitch, the lower the amount of radiation dose delivered. Pitch optimization should be discussed with the manufacturer’s CT Applications Specialist. Ideally, pitch should be greater than 1.
Create Limitations on Double Scans and Multi-Phase Studies: Whenever possible, eliminate studies without contrast because no-contrast scans often provide little additional diagnostic information and actually increase patient dose and overall exam cost. You should also consider eliminating no-contrast scans in multi-phase examinations for the same reasons.
Iterative Reconstruction Hardware & Software / SafeCT: Iterative Reconstruction (IR) is the newest method of CT image reconstruction. It’s a highly effective method of reducing image noise and also has the ability to routinely reduce patient dose by 40% to 50%. SafeCT is a major component in an overall CT dose management solution. SafeCT Iterative Reconstruction should be employed with “Smart CT Protocols” such as kVp changes, automatic dose modulation (auto-mA), limited scan coverage and multi-phase considerations etc. in order to optimize dose savings.
Comprehensive CT Dose Management Implementation requires:
• Dedicated, committed and focused leadership
• All members of the organization need to agree that CT dose reduction is a major goal.
• All CT acquisition protocols must be examined and revised to focus on radiation reduction.
• The process requires a team consisting of a lead CT Radiologist, lead CT Technologist and vendor CT Application Specialists
• A continuous feedback loop and processes must be in place to educate staff members and to audit each CT scanner’s compliance.
A unified commitment to a cohesive strategy is the first and most important step in reducing radiation doses.